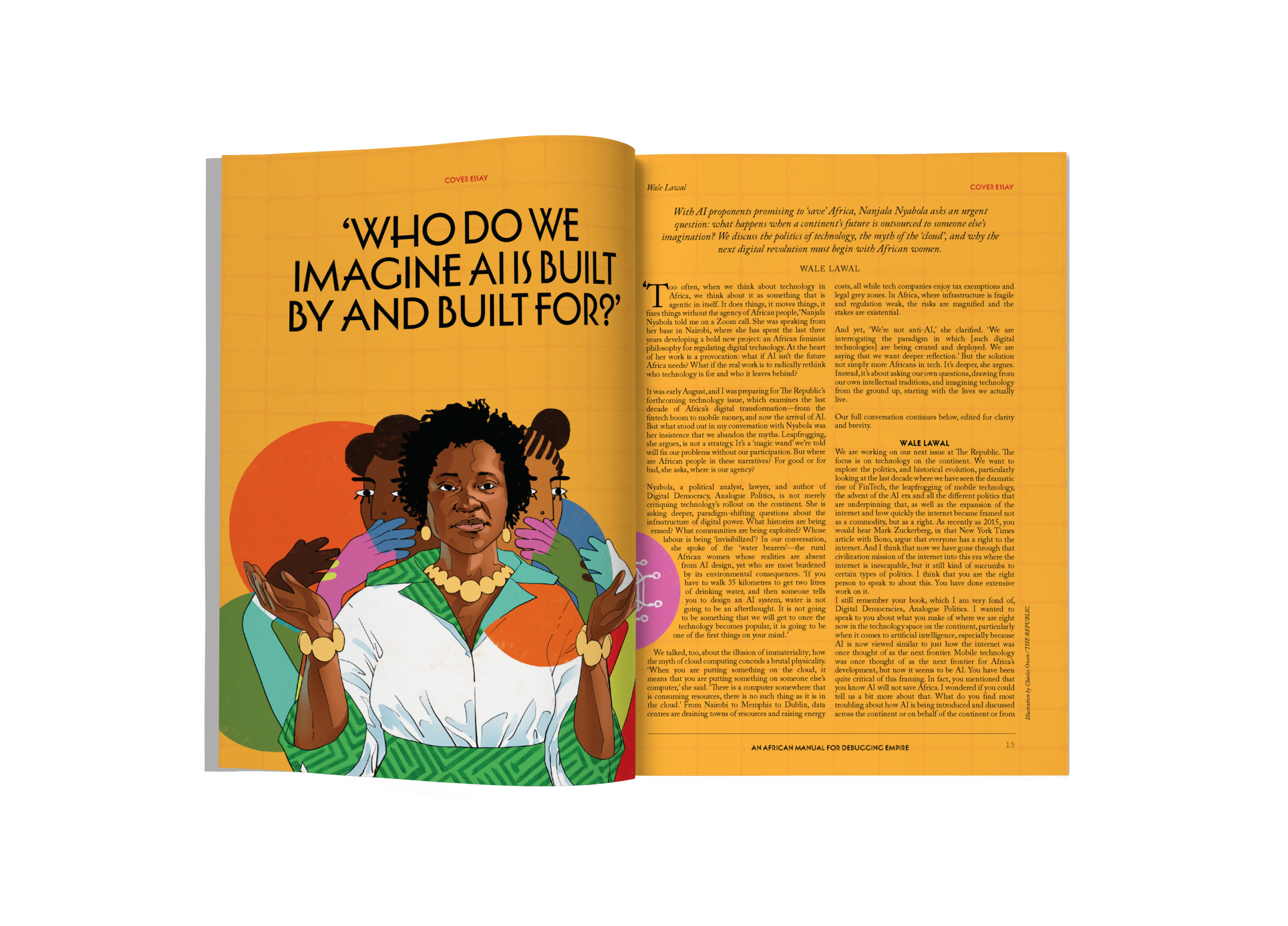
Illustration by Charles Owen / THE REPUBLIC.
THE MINISTRY OF HEALTH
Africa’s AI Path to Health Impact

Illustration by Charles Owen / THE REPUBLIC.
THE MINISTRY OF HEALTH
Africa’s AI Path to Health Impact
A robot, Osadebe, came out to greet me. Osadebe would be performing my procedure and had already been synced to all my records in The Database. Osadebe knew my favourite musicians, my favourite books, and even made jokes that matched my sense of humour. I couldn’t believe it. Osadebe would be something of a nurse and physical therapist to me after performing my procedure. Osadebe had already created customized versions of recommended lifestyle changes for me, accounting for my quirks—like what time I liked to go to sleep and how flavourful I liked my food. Osadebe would also be calling me to make sure I was fine before and after the procedure and providing me some counselling if needed.
—‘The Winged Woman’ by Ebele Mogo
In 2021, in response to a call for speculative fiction on alternative economic futures and technologies by Edgeryders, I wrote the short story ‘The Winged Woman’. It envisioned a future where an AI agent, Osadebe, trained on biomedical data, supported a woman preparing for surgery, offering personalized diagnostics and emotional support. At the time, it seemed like science fiction from a distant future. Yet, only a few years later, that future no longer seems so distant. By 2024, the United States Food and Drug Administration had authorized over 880 AI-powered medical devices, ranging from diagnostic tools and radiology image interpreters to systems that predict deterioration or guide treatment pathways. Algorithmic agents are already helping people plan surgeries, support diagnoses, and translate complex health information, and the promise of surgical robots is very real.
In 2020, I led a team of volunteers in a distributed effort to rapidly translate the World Health Organization’s COVID-19 guidelines into multiple African languages. We onboarded translators, built a workflow, created quality assurance protocols for translation into 18 languages, and disseminated the content in under three weeks. It was a human-powered and agile response to linguistic gaps in the middle of a global emergency. In a few years, the launch of ChatGPT would accelerate the global adoption of Large Language Models. Today, a fair pass at those translations could be generated in minutes, at least for the widely represented languages.
We are at the threshold of agentic AI, models capable of goal-directed behaviour, autonomous initiative, and reasoning in constrained environments. The pace of advancement is disorienting, such that benchmark evaluations that once seemed reliable now lag behind models that evolve week to week. This gap creates challenges in how we measure real-world performance.
THE POSSIBILITY OF PRECISION
Science’s computational turn is fully underway. In 2020, DeepMind’s AlphaFold revolutionized biology, solving the longstanding puzzle of protein folding. Almost overnight, researchers gained the ability to predict the 3D structure of virtually any protein. The impact was immediate and profound, speeding up vaccine development and offering new insights into complex diseases.
In public health, advances in computation are reshaping how needs are detected, predicted and addressed. During the pandemic, my colleagues and I used social media analytics to understand how Nigerians in cities were experiencing the first COVID-19 lockdowns. The analysis revealed how people were coping, the challenges they faced with lockdown measures, and the voices shaping the health narrative at the time. These trends offered early indicators of unmet needs, though shaped by who was online, primarily urban populations with greater connectivity.
For instance, while public health authorities struggled to maintain reach and visibility, influencer accounts like Chinonso Egemba @aproko_doctor played an outsized role in driving engagement, filling the vacuum, and shaping public understanding in real time. This divergence reinforced an insight: public sentiment and behaviour can be explored and used to tailor interventions and inform policy with relatively lightweight data inputs.
More recent applications show just how deep the possibility for precision can go. A 2025 publication in Frontiers in Genomics combined social, environmental and genomic data to determine why malaria risk varied among people living in the same geographic area in Brazil. This level of granularity suggests a future where health systems can intervene proactively before outbreaks occur, at the level of local government areas or perhaps even households.
If messaging, interventions and resources can be tailored at this level, public health could potentially shift from reactive to proactive. We can move beyond generalized guidelines to systems that respond to specific contexts, considering who is at risk, why, and what would make a difference in real time. Rather than waiting for cases to rise, systems can learn from existing patterns and act preventively, allocating resources more efficiently. It also offers the possibility of higher adherence, precisely because interventions are more relevant to the people they aim to serve.
Importantly, this also enables feedback loops: outcomes inform future action, and public health is continuously refined in response to how people actually live, move and respond. This is the heart of precision public health. With global health budgets tightening, the argument for precision is also economically compelling. Targeted prevention consistently delivers strong returns on investment. The capabilities are expanding rapidly, but realizing their full potential requires building on the lessons from Africa’s first digital health wave.
shop the republic
-
‘The Empire Hacks Back’ by Olalekan Jeyifous by Olalekan Jeyifous
₦70,000.00 – ₦75,000.00Price range: ₦70,000.00 through ₦75,000.00 -
‘Make the World Burn Again’ by Edel Rodriguez by Edel Rodriguez
₦70,000.00 – ₦75,000.00Price range: ₦70,000.00 through ₦75,000.00 -
‘Nigerian Theatre’ Print by Shalom Ojo
₦150,000.00 -
‘Natural Synthesis’ Print by Diana Ejaita
₦70,000.00 – ₦75,000.00Price range: ₦70,000.00 through ₦75,000.00
DEJA VU
Africa’s first digital health wave arrived with ambition. SMS interventions, mobile diagnostics and app-based services promised to expand access, promote behaviour change and democratize care. By 2020, mobile network coverage had reached nearly 90 per cent of the continent, fuelling a surge in mobile health platforms. In Gabon, mobile money transfers were briefly used to fund universal health coverage. In Rwanda, partnerships with international organizations expanded digital health access into rural zones. For a moment, it seemed digital health might outpace the systemic barriers that had long constrained public health delivery.
Yet progress was also deeply uneven. While tertiary hospitals in urban centres adopted electronic health records, rural clinics struggled with inconsistent electricity, poor connectivity and overburdened staff. In Nigeria, for instance, while Lagos-based startups were digitizing tertiary hospitals, many rural health centres still operated without reliable power, much less digital infrastructure. Shifts in political leadership routinely disrupted funding streams and unravelled fragile public-private partnerships. The deeper lesson was about implementation: infrastructural gaps, fragmented efforts, and donor-driven cycles left many digital initiatives stuck at the pilot stage, disconnected from the public health institutions they aimed to strengthen. Thus, promise, in many cases, remained just that.
These divides reflect not just access, but a deeper question of inclusion in innovation design. Our review of 54 studies on natural language processing for health across Africa revealed a rich array of applications, such as chatbots for vaccine uptake, tools for misinformation detection, summarization of epidemiological data, and more. The breadth of applications was notable, revealing a fertile space of experimentation. Yet, it revealed patterns that mirrored the 2010s digital health boom: most innovations stalled at prototype stages, with limited evidence of full deployment. Only a handful showed pathways for alignment with national health infrastructures, and even fewer reflected participatory or community-led design. Without real-world testing and outcome tracking, it was difficult to assess the true value of these tools in real-world settings.
Language coverage also highlighted structural limitations. English accounted for 74 per cent of Natural Language Processing (NLP) tools, while widely spoken African languages like Igbo, Swahili and Yoruba remained underrepresented. This limited reach is particularly striking given the importance of language in public health messaging. Once again, the pattern repeats: exciting tools, but without integration, funding, or alignment with national health priorities.
Benchmarks, standardized tests used to evaluate a model’s performance, often focus on general capabilities like reading comprehension, commonsense reasoning or statistical logic. While useful in broader AI research, these metrics rarely capture the complexities of health planning and service delivery. As a result, models may excel on paper but underperform in real-world scenarios. The strengths of general-purpose language models can even become limitations in domain-specific contexts such as HIV programme design, where deep contextual understanding is critical. Meanwhile, open-source alternatives that could be adapted for local relevance often demand computational resources far beyond what many low and middle-income countries can support.
shop the republic
TOWARD THE FUTURE
As we build the next generation of health technologies, we must ask ourselves: What does true impact look like? This time, we can build with the benefit of hindsight and widen our lens as we do so. If computational tools are to move beyond isolated success stories, they need to be deliberately integrated, governed, and evaluated as part of a broader population health infrastructure.
Precision is often imagined narrowly as clinical personalization, matching treatments to patients based on unique biology. However, what distinguishes precision medicine from precision public health is the promise of prevention at scale and the population as the unit of interest. Realizing that promise requires robust data architecture, systems capable of integrating multifaceted signals, and translating them into timely, actionable insights for entire populations.
Africa is building a foundation for this kind of precision. In Nigeria, for example, the African Centre of Excellence for Genomics of Infectious Diseases (ACEGID) has become a continental leader, providing real-time pathogen surveillance and data that inform population-level responses. ACEGID’s work under the H3Africa initiative, a major pan-African genomics research program launched in 2010 to build genomic infrastructure and capacity across Africa, has expanded genomic infrastructure and training across the continent, making Nigeria a key site for Africa-led genomic science. These efforts represent a broader Nigerian momentum in health innovation, though realising their full potential will require sustained institutional support and integration into national systems.
Strategic coordination is also beginning to emerge at the policy level. The African Union’s 2024 Artificial Intelligence Strategy offers a continent-wide vision for sovereign digital ecosystems. It encourages investment in interoperable data infrastructure and regional collaboration to standardise data governance practices. It also emphasises African ownership of innovation processes and highlights the importance of aligning AI development with public priorities, including health system resilience and responsiveness. Though still early in its implementation, the strategy has catalysed continental policy dialogues with member states on framing and adapting national AI roadmaps to prioritise public interest applications, including health.
Oversight also remains essential. Our evaluation of Swahili machine translation applied to health use cases found that 19 of 71 outputs were considered harmful or misleading. Language, context and cultural nuance cannot be fully captured by models trained on scraped internet text, particularly for underrepresented languages and domains. Human-in-the-loop systems will thus need to continue to provide grounding and accountability, even as automation advances. Masakhane, the grassroots NLP collective, offers an example of how this oversight can be integrated from the start.
The path to impact also requires robust, outcome-centred evaluations that move beyond AI-specific metrics or usability studies. An overreliance on metrics like accuracy, precision, F1-score and recall, while useful for benchmarking model performance, says little about whether tools work in real-world settings or meaningfully improve health. Tools must also be assessed for whether they lead to better care delivery, improved behaviour, or measurable health gains. Where formal AI evaluation is still emerging, best practices from digital health can guide the way. For example, the WHO’s Monitoring and Evaluating Digital Health Interventions framework offers structured guidance that can be adapted to AI contexts.
Examples from other emerging settings provide instructive examples of how data systems can be built modularly, laying the groundwork for scalable, context-aware AI in health. Consider India’s Ayushman Bharat Digital Mission. Rather than relying on cloud-based systems that store all data centrally and require constant internet access, the mission uses a federated architecture. In this model, data is stored locally at the clinic or hospital level and connected through standardised APIs. Patients can manage access to their data through a consent manager. This approach allows facilities with limited connectivity to continue operating and later sync data when possible. It also enables national planning through aggregated, anonymised insights without compromising individual privacy.
Ethiopia’s HEP Assist offers a similarly instructive model for resource-constrained settings. Designed to support frontline Health Extension Workers, the platform provides real-time, step-by-step guidance for screening, diagnosis, and referral decisions across key services like maternal care, child health and infectious disease management. Workers input basic patient information into the mobile application, which then uses built-in clinical protocols to suggest next steps, such as whether a patient should be referred to a higher-level facility or monitored at home. Crucially, the platform functions offline and synchronizes when connectivity becomes available, allowing continuous service delivery even in remote areas. By reducing uncertainty and standardizing care processes, HEP Assist enables more consistent, timely, and appropriate decision-making at the frontlines.
shop the republic
THE STAKES ARE MOUNTING
Public health emergencies are becoming more frequent, complex and protracted. Many unfold in regions where infrastructure is already stretched, and the economic impact of illness can be catastrophic. More than a billion people still face the threat of being pushed into poverty by healthcare costs alone. Without intentional transformation, systems meant to protect life may be overwhelmed by the very crises they are meant to contain. These challenges are compounded by shrinking global health funding. This makes the economic case for precision even more urgent, as we cannot afford to waste resources on poorly targeted interventions.
This article began with Osadebe, a fictional AI health worker capable of guiding patients with empathy, insight, and cultural fluency. What if Osadebe were more than a clinical assistant? Imagine them embedded within a broader system that could detect genomic signals linked to chronic disease risk, interpret mobility data for signs of food insecurity, and use climate trends to forecast vector-borne outbreaks? What if they could help allocate resources dynamically, coordinate across clinics and communities, and adapt in real time? Tools like Osadebe could recommend interventions, send reminders, adjust care plans, and collaborate with public health officials to redirect resources, not just to optimise treatment, but to keep people well. Just as importantly, Osadebe could support long-term behaviour change, not through generic messaging, but through culturally grounded engagement that makes prevention actionable. The future of public health lies in building systems that can learn, adapt and act—not just to treat illness, but to prevent it altogether⎈
BUY THE MAGAZINE AND/OR THE COVER
-
‘The Empire Hacks Back’ by Olalekan Jeyifous by Olalekan Jeyifous
₦70,000.00 – ₦75,000.00Price range: ₦70,000.00 through ₦75,000.00 This product has multiple variants. The options may be chosen on the product page -
The Republic V9, N3 An African Manual for Debugging Empire
₦40,000.00
US$49.99